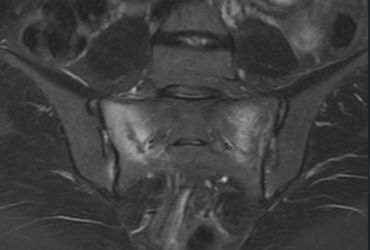
Whilst severe pelvic fractures are treated by orthopaedic surgeons in trauma centres, spontaneous sacral insufficiency fractures might be treated by endocrinologists, or rehabilitation physicians. But here are my comments!
Continue readingRecliners after Surgery?
After surgery, sitting causes blood to sit in your leg veins, with a risk of clotting, it’s better to have your legs up!
Continue readingOperative or Non-operative Care of Achilles Rupture
Robotic knee replacement surgery has been widely available for some years – and in Ballarat at St John of God, we have three robots to use with three different companies total knee replacement, and some partial knee replacements. Our surgeons using it find it a useful tool streamlining the operation.
Continue readingAdvances in Knee Replacement – Is the robot helping?
Robotic knee replacement surgery has been widely available for some years – and in Ballarat at St John of God, we have three robots to use with three different companies total knee replacement, and some partial knee replacements. Our surgeons using it find it a useful tool streamlining the operation.
Continue readingAOANJRR milestone – one million hip replacements recorded
The Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR) has officially recorded its one millionth hip replacement procedure.
Continue reading